Written by Caiden McPherson; published February 27, 2025
Osteoporosis, Osteopenia, and Bone Health
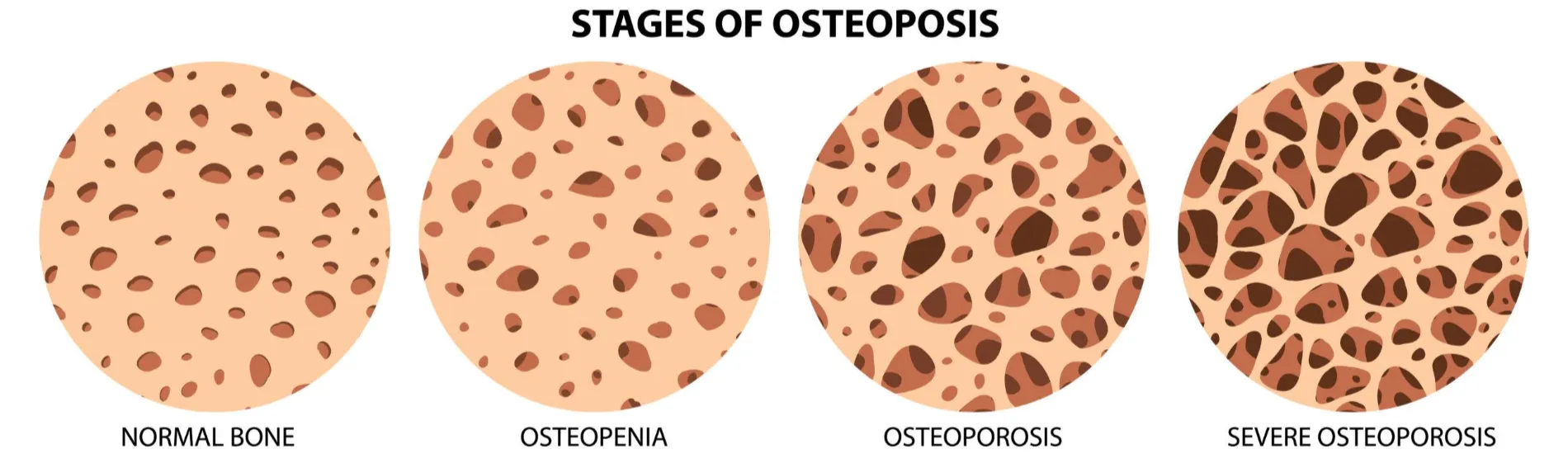
Diseases that affect bone health have far-reaching implications, negatively impacting hbmultiple areas of life. Osteoporosis and osteopenia are two of the most common skeletal disorders in older adults. Osteoporosis is a condition in which bone reabsorption exceeds bone remodeling, leading to porous, fragile bones that are prone to fracture (Rowe, 2023). These porous fragile bones are characterized by low bone density, a hallmark of the disease. Osteopenia, a precursor to osteoporosis, is characterized by decreased bone mineral density, however the decrease seen in osteopenia is not as severe as the decrease seen in osteoporosis (Varacallo, 2023). Both conditions increase the likelihood of bone fracture, especially after a fall.
Fractures related to osteoporosis and osteopenia occur more than most realize. A peer-reviewed study published in 2016 revealed that across Europe and the United States, 40% of postmenopausal women and 30% of men will experience an osteoporotic fracture (Sozen, 2016). These fractures can significantly impact independence and quality of life, and create financial strain due to hospitalization and rehabilitation costs. Additionally, the fear of falling is a significant cause of anxiety in older adults, often leading to increased inactivity and further bone density loss (Bae, 2023). Given the widespread prevalence of osteoporosis, extensive research has been conducted on its prevention and management. Exercise programs crafted by certified physical therapists have proven to be valuable treatment options, leading to reduction in bone mineral loss and fall risk.
Exercise and it’s Effect on Osteoporosis and Osteopenia
The ability of exercise to prevent and manage osteoporosis lies in the mechanism of bone development. Bone remodeling follows a principle known as Wolff’s Law, which states that the more mechanical loading — or physical force — applied to a bone through muscle and tendon activity, the more the bone will mineralize in the loaded area (Rowe, 2023). Clinical studies have demonstrated that exercise programs — especially those tailored to the individual by a certified physical therapist — can increase bone mineral density in key areas where osteoporotic fractures commonly occur, such as the lumbar spine and the hip (Hartley, 2022). In contrast, immobilization and low levels of physical activity are significant contributors to osteoporosis, as bones fail to receive the stimuli needed for growth and mineralization. Lifelong exercise decreases the risk for developing osteopenia and osteoporosis, but once an individual is diagnosed with osteoporosis, exercise is still a useful tool for managing the condition and preventing falls.
Exercise is not the only factor that contributes to the development of osteopenia and osteoporosis. Bone health is also heavily influenced by estrogen levels. In postmenopausal women, estrogen declines, leading to a decrease in bone remodeling and placing them at the highest risk for osteoporosis and osteoporotic fractures (Rowe, 2023). Because of this, osteoporosis prevention strategies are crucial for postmenopausal women, although men can also develop the disease. Other risk factors that contribute to osteoporosis include alcohol abuse, smoking, high salt intake, and Vitamin D and/or calcium deficiencies (Sozen, 2016). Addressing these risk factors and following an exercise program created by a physical therapist can effectively manage osteoporosis and reduce the risk of fractures.
The Role of Physical Therapists in Prevention and Management
Certified physical therapists play a vital role in helping individuals manage osteopenia and osteoporosis to prevent falls and fractures. The Journal of Geriatric Physical Therapy provides guidelines on how physical therapy can be used to treat and prevent osteoporosis across various patient populations, including premenopausal and postmenopausal women at high risk, as well as men at risk for developing osteoporosis (Hartley, 2022). Among the most effective interventions are resistance training and weight-bearing exercises.
Resistance training strengthens muscles and places beneficial mechanical load on bones, promoting bone density maintenance. It includes both external resistance exercises—such as free weights or resistance machines—and bodyweight exercises like push-ups. A meta-analysis found that exercise prescriptions incorporating resistance training, along with weight-bearing activities like jogging, walking, or stair climbing, helped slow bone mineral density loss in areas prone to osteoporotic fractures (Hartley, 2022). Another meta-analysis highlighted that resistance training combined with impact-based activities—such as jumping, stomping, and even impact-heavy dance styles like Zumba—also contributed to reduced bone loss (Bae, 2023). The mechanical strain produced by these exercises is a key factor in preventing further bone deterioration. By following a physical therapist-prescribed exercise plan, individuals can significantly reduce their risk of falls and fractures.
Because strength, balance, and mobility levels vary between individuals, customized exercise plans are essential in preventing injury. Many older adults express concerns about exercising due to fear of injury (Hartley, 2022). Physical therapists are trained to assess fall risk and prevent injury when prescribing exercise. Additionally, physical therapists help guide clients through exercise and demonstrate healthy adaptations to make exercise accessible and beneficial to people of all ages and abilities. Physical therapists use clinical reasoning to develop personalized exercise programs that help manage osteoporosis, address barriers to exercise, and ensure safety.
Financial barriers can also discourage participation in regular exercise. Some older adults cite gym membership costs as a challenge to maintaining a fitness routine (Hartley, 2022). Physical therapists can recommend and demonstrate effective at-home exercises that require minimal or no equipment, making osteoporosis management more accessible and affordable. Physical therapists provide valuable insight that can help individuals managing osteoporosis do so in a way that is safe, affordable, and sustainable.
In Summary
Osteoporosis and osteopenia are common conditions that increase fracture risk and can significantly impact quality of life. Fractures from osteoporosis lead to pain, financial strain, and can result in decreased independence. Furthermore, osteoporosis-related anxiety about falls and injuries can lead to decreased activity, further exacerbating bone loss. Individualized exercise programs are clinically proven to increase strength and reduce decline in bone mineral density, leading to reduced risk of fractures and falls alike. With the guidance of a certified physical therapist, individuals can effectively manage osteoporosis and osteopenia, reducing the likelihood of fractures and falls.
At Synergy Physical Therapy and Wellness, we are committed to providing holistic care that benefits both body and mind. Our physical therapists use clinical reasoning and evidence-based practices to promote the health and well-being of our clients and community. If you or a loved one is experiencing inactivity or anxiety related to osteoporosis, osteopenia, or an injury, call today to receive individualized care that will help you live your best life!
Works Cited:
Bae S, Lee S, Park H, Ju Y, Min SK, Cho J, Kim H, Ha YC, Rhee Y, Kim YP, Kim C. Position Statement: Exercise Guidelines for Osteoporosis Management and Fall Prevention in Osteoporosis Patients. J Bone Metab. 2023 May;30(2):149-165. doi: 10.11005/jbm.2023.30.2.149. Epub 2023 May 31. PMID: 37449348; PMCID: PMC10345999.
Hartley, G. W., Roach, K. E., Nithman, R. W., Betz, S. R., Lindsey, C., Fuchs, R. K., & Avin, K. G. (2022). Physical Therapist Management of patients with Suspected or Confirmed Osteoporosis: A Clinical practice guideline from the Academy of Geriatric Physical Therapy. Journal of Geriatric Physical Therapy, 44(2), E106–E119.
Rowe, P., Koller, A., & Sharma, S. (2023, March 17). Physiology, bone remodeling. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499863/
Sozen, T., Ozisik, L., & Basaran, N. C. (2016). An overview and management of osteoporosis. European Journal of Rheumatology, 4(1), 46–56. https://doi.org/10.5152/eurjrheum.2016.048
Varacallo, M. A., Seaman, T. J., Jandu, J. S., & Pizzutillo, P. (2023, August 4). Osteopenia. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499878/
image retrieved from freepik.com
